Risk Factors in Breast Cancer
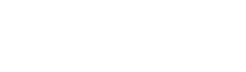
Breast Cancer Risk Factors
Some factors greatly affect the risk of breast cancer, which cannot be changed. For example, the most important risk factors for breast cancer are being a female and senescence, however there are other factors that slightly increase the risk of breast cancer that you may be able to control. For instance, healthy lifestyle may help reduce the risk of breast cancer. Being aware of influencing risk factors may alleviate any concerns and motivate people to undergo a suitable breast cancer screening plan.
Schematic of Breast Cancer Risk Factor
- Being a female is the main risk factor for breast cancer. Although men can also develop breast cancer, it is about 100 times more common in women.
- Age is a risk factor for breast cancer in women and men. The older a person is, the more likely they are to develop breast cancer.
Age of onset of menstruation and menopause
Early menstruation and late menopause increase the risk of breast cancer. Starting menstruation at a young age is associated with a slightly increased risk of breast cancer.
Age of first pregnancy
Firstly, it is necessary to mention that the meaning of pregnancy here is the complete period of 9 months of pregnancy, regardless of whether it leads to the birth of a live baby or not. Age over 35 years at the first pregnancy increases the risk of breast cancer by 40% as compared to women whose first pregnancy was at the age of 20. On the other hand, when the age of the first pregnancy is lower, the risk of breast cancer is also relatively lower.
Alcohol and smoking

Drinking alcohol increases the risk of breast cancer. For example, women who drink 2-3 alcoholic drinks per day have a 20% increased risk of developing breast cancer as compared to women who do not drink alcohol. Alcohol consumption increases the serum level of estradiol.
Many studies have been conducted on the relationship between smoking and the increased risk of breast cancer. In some of these studies, smoking during adolescence and puberty, when the breast tissue is more sensitive to carcinogens, has been associated with an increased risk of breast cancer.
Genetics

About 5-10% of breast cancers have a genetic background. Many of cases with breast cancer have the mutated genes called BRCA1 and BRCA2, which increases their risk of developing breast and ovarian cancers or breast cancer alone. In cases where breast cancer occurs in family members before the age of 40, or there is a history of the disease in men close to the family, or there is a history of ovarian cancer in the person herself or his family, genetic counseling is strongly recommended.
Family history of breast cancer

Among the factors known to increase the risk of breast cancer, family history is considered as one of the most important factors. About 5-10% of breast cancers are caused by a family history, and it is estimated that 13-16% of women with breast cancer have at least one of their family members (mother, sister or daughter) with cancer. A woman who has a family member with breast cancer is almost at twice higher risk as a woman without this family history. If she has more than one female family members with history of breast cancer, her risk increases by 2-4 times.
The lower the age of the family member of a person, the more likely the risk is. For example, a woman whose mother was diagnosed with breast cancer before age 40 has almost twice the risk as someone without a history. For a woman whose mother is diagnosed at an older age, the increasing risk is not so great.
Hormones consumption
Estrogens are natural hormones that are important in sexual development and other body functions. Higher levels of estrogen in the blood are associated with an increased risk of breast cancer in postmenopausal women.
Before menopause, most estrogens are produced in the ovaries. After menopause, the ovaries no longer produce much estrogen, and estrogens mainly come from fat tissue. Higher levels of estrogen in the blood are associated with an increased risk of breast cancer in postmenopausal women. Researchers are studying the possible link between premenopausal breast cancer and estrogen.
Postmenopausal therapeutic hormone (estrogen plus progesterone) is approved by the Food and Drug Administration for short-term relief of menopausal symptoms, but should be prescribed with the doctor's opinion and in necessary cases. This hormones are not usually given to breast cancer survivors because it may increase the risk of recurrence. All women can lower their estrogen levels by:
- Maintaining a healthy weight after menopause
- Physical activity (exercise)
Prolactin is a natural hormone that plays a role in breast growth and milk production during breastfeeding. The risk of breast cancer is slightly higher in women with higher prolactin levels than in women with lower levels.
The relationship between female hormones and breast cancer can be investigated in different ways:
- Hormone replacement therapy after menopause
- Hormonal treatments after breast cancer
- Use of female hormones to prevent pregnancy
Taking contraceptives
Previous studies have shown that there is a delicate relationship between the use of birth control pills and the increased risk of breast cancer. Especially in young women who have used these drugs for a long time and women who have used these pills before their first pregnancy, they have a 20-30% higher chance of developing breast cancer.
Current or recent use of birth control pills slightly increases the risk of breast cancer, and women are 30% more at risk of breast cancer.
BMI body mass index (weight)
Studies show that there is a relationship between body mass index (which is related to the ratio of weight to height) and the risk of breast cancer. However, this index affects the risk differently before and after menopause. Being overweight or obese after menopause increases the risk of breast cancer. It seems that the possibility of breast cancer increases in obese women during birth giving (weight of female). For people of ages 20 years and older, weight status categories are:
Body mass index:
5/18 to 9/24 = normal
25 to 9.29 = overweight
30 and above = obese
Lactation and density of breast tissue

Breastfeeding reduces the risk of breast cancer, especially premenopausal breast cancer. The preventive effect of breastfeeding in premenopausal breast cancer is more obvious. It is said that the longer the duration of breastfeeding, the stronger the protective effect, especially if this period is longer than 6 months. However, the lack of milk or non-secretion in some women, leading to the reduction of the breastfeeding period to less than 6 months, has no effect on the occurrence of breast cancer. Also, stopping milk by using hormonal drugs does not increase the risk of breast cancer, but if the mother's age at the time of breastfeeding is lower, this protective effect will be greater. Altogether, since breastfeeding is not very common among mothers in western countries, this issue requires wider investigations in Iran.
Breast tissue density
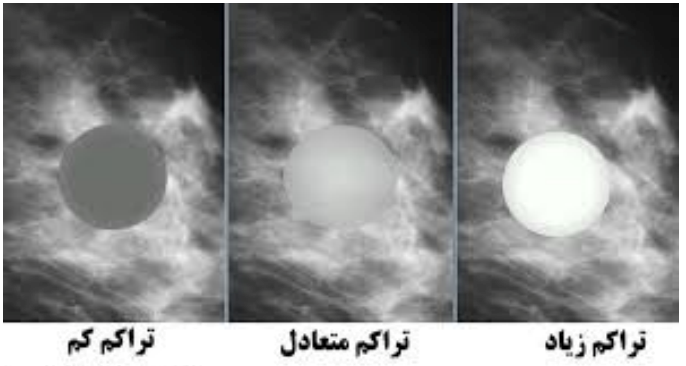
Breast tissue density is a measure used to describe the ratio of different tissues of female breasts. It compares the breast area and the connective tissue seen in the mammogram with the fat area.
Women with breast density are affected 4-5 times more often than women with low breast density. Compared to women with low bone density, women with high bone density are about 60-80% more at risk of breast cancer, which seems to be the cause of the high level of estrogen in their body.
Exercise (Physical activity)

The risk of breast cancer is lower in women who exercise regularly (physical activity) as compared to women who are not exercising. When reviewing the evidences, regular exercise appears to reduce the risk of breast cancer by 10-20%. This advantage is clearly seen in postmenopausal women.
Constant night shift work
Women who usually work night shifts for years have a slightly increased risk of breast cancer. More research is needed to determine what aspects of shift work may affect breast cancer risk. One possible reason for the increased risk among these people is exposure to light at night.
Lobular carcinoma in situ (LCIS) disease
When abnormal cells grow inside the lobules of the breast, but do not spread to adjacent tissues or beyond, this disease is called noninvasive lobular carcinoma (LCIS).
Although the term LCIS includes the word "carcinoma," but it is not cancer. However, LCIS increases the risk of developing breast cancer. As compared to women without LCIS, women with LCIS are 7-11 times more likely to develop invasive cancer.
Exposure to extensive radiation
High exposure to X-rays early in life, such as radiation therapy to the chest for lymphoma, increases the risk of breast cancer. For example, women treated with radiation therapy to the chest for Hodgkin's disease at a young age have a 3-7 times higher risk of developing breast cancer compared to women who had Hodgkin's disease at a younger age, but never received radiation therapy. Very low doses of radiation (such as mammography x-rays and other medical imaging) do not have a large effect on the risk of breast cancer.
During the clinical examination, if any of the following symptoms are present, inform the doctor:
- A hard lump or lump
- An old lump that has gotten bigger
- Hard lump or thickening inside the breast or armpit area
- Recent enlargement of one breast and infertility
- Swelling, warmth, redness or darkening of the breast
- Change in breast size or shape
- Orange skin of the breast
- Dimpled or flaky skin, itching, scaly sores, or rashes on the nipple
- Pulling the nipple or other parts of the breast inward
- Nipple discharge that suddenly and spontaneously from a duct and breast
- New onset of pain in one spot that does not go away
To get more information on nutrition, you can visit the Clinics of Motamed Cancer Institute ACECR or contact the numbers below.
Consultant contact number: 021-66404020 / 09124885127
References:
· Breast cancer facts & figures 2019-2020
· Komen.com/about breast cancer/risk factors
Compiled, written and translated by:
Dr. Ahmad Fazilat
Faculty member, Dept of Genetics, Motamed Cancer Institute, ACECR